Treatment Overview
Carotid artery stenting is a procedure to open a narrowed carotid artery. There is a carotid artery on each side of the neck. They supply blood to the brain.
Fatty buildup can narrow these arteries. This buildup is called plaque. When one or both of your carotid arteries are narrowed, it can make it hard for blood to flow to the brain. This buildup also raises your risk of stroke. This procedure may improve blood flow to your brain and lower your risk of having a stroke.
You will get medicine to prevent pain and help you relax. The doctor will put a small tube into a blood vessel in your groin or arm. This tube is called a catheter. The doctor will move it through the blood vessel to your carotid artery. Then the doctor will put dye into the catheter. The dye will make your carotid artery show up on X-ray pictures. This lets the doctor find the narrow section of the artery.
The catheter is used to move a balloon and an expandable tube, called a stent, into the artery. The balloon is placed inside the stent and inflated. This opens the stent and pushes it into place against the artery wall. The balloon is then deflated. The doctor will take out the balloon and catheter from your body. The stent will stay in your artery. After time, the cells lining the blood vessel will grow through and around the stent to help hold it in place.
The procedure usually takes about 1 to 2 hours. You may need to stay in the hospital for 1 or 2 days after the procedure.
How It Is Done
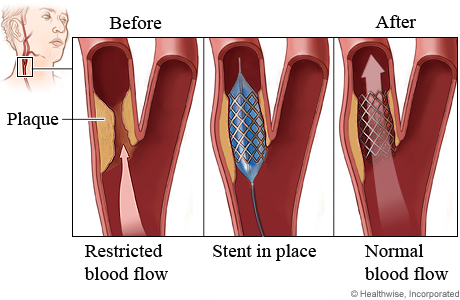
During carotid artery stenting, a small, expandable tube called a stent is permanently inserted into the carotid artery.
To insert the stent, the doctor uses another tube called a catheter. The doctor inserts the catheter into a blood vessel in your groin or arm and moves it to the carotid artery.
A very thin guide wire is inside the catheter. The guide wire is used to move a balloon and the stent into the carotid artery. The balloon is placed inside the stent and inflated. This opens the stent and pushes it into place against the artery wall. The balloon is then deflated and removed, leaving the stent in place. After time, the cells lining the blood vessel will grow through and around the stent to help hold it in place.
What To Expect
You may need to stay in the hospital for 1 or 2 days after the procedure.
After you leave the hospital, you may notice a bruise or small lump where the catheter was put in. This is normal and will go away. The area may feel sore for a few days. You can do light activities around the house. But don't do anything strenuous until your doctor says it's okay. This may be for at least several days.
You will take medicines to help prevent a stroke. You will still need to have a heart-healthy lifestyle. This lifestyle includes eating healthy foods, being active, staying at a healthy weight, and not smoking. This will give you the best chance for a longer, healthier life.
You will have regular tests to check blood flow in your carotid arteries.
Why It Is Done
Carotid artery stenting is done to help lower your risk of stroke.
Your doctor may recommend this procedure based on certain things. These include:footnote 1, footnote 2, footnote 3
- The amount of narrowing (stenosis) in your carotid arteries. A procedure may be an option if the narrowing is 50% or more.
- Whether you had a stroke or TIA within the past 6 months. If you have not had a stroke or TIA, it is less clear that the procedure will help you.
Learn more
How Well It Works
If you have not had a TIA or stroke
For people who have not had a stroke or TIA, it is not clear when stenting might be a good choice. Stenting may help prevent a stroke in the long run. But in the short run, it increases the risk of stroke and death. Medicine and a heart-healthy lifestyle may work as well as stenting to prevent a stroke, and they don't have the risks of stenting.
Carotid artery stenting may be an option if you have more than 70% narrowing and you have a low risk of serious problems from stenting.footnote 1, footnote 3
It is not clear that stenting will reduce your stroke risk more than medicines and a heart-healthy lifestyle. Studies are being done to compare current medical therapy with stenting.
If you have had a TIA or stroke
Carotid artery stenting can help lower your risk of stroke if your carotid artery is narrowed by 50% or more. footnote 2, footnote 3
You may benefit most from stenting if it is done within 2 weeks of the stroke or TIA.footnote 2, footnote 3
Risks
The risks of carotid artery stenting include:
- Infection.
- Bleeding at the catheter insertion site.
- Damage to the blood vessel at the catheter insertion site.
- Stroke, heart attack, or death.
- The artery can narrow again.
The risks of a procedure depend on things like your age and your overall health.
References
Citations
- Meschia JF, et al. (2014). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, published online October 28, 2014. DOI: 10.1161/STR.0000000000000046. Accessed October 29, 2014.
- Kleindorfer DO, et al. (2021). 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7): e364–e467. DOI: 10.1161/STR.0000000000000375. Accessed June 4, 2021.
- AbuRahma AF, et al. (2021). Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. Journal of Vascular Surgery, published online June 19, 2021. DOI: 10.1016/j.jvs.2021.04.073. Accessed July 19, 2021.
Credits
Current as of: July 31, 2024
Meschia JF, et al. (2014). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, published online October 28, 2014. DOI: 10.1161/STR.0000000000000046. Accessed October 29, 2014.
Kleindorfer DO, et al. (2021). 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7): e364–e467. DOI: 10.1161/STR.0000000000000375. Accessed June 4, 2021.
AbuRahma AF, et al. (2021). Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. Journal of Vascular Surgery, published online June 19, 2021. DOI: 10.1016/j.jvs.2021.04.073. Accessed July 19, 2021.